Exploring the Risk of Ovarian Cancer after Total Hysterectomy

The Importance of Understanding Ovarian Cancer Risk Factors
When it comes to women's health, the risk of developing ovarian cancer is a significant concern. Ovarian cancer is the fifth most common cancer among women and is often referred to as the "silent killer" due to its difficult-to-detect symptoms in the early stages.
For women who have undergone a total hysterectomy, a surgical procedure that involves the removal of the uterus and cervix, understanding the risk of developing ovarian cancer becomes even more crucial. In this informative article, we will shed light on the risk factors associated with ovarian cancer post-total hysterectomy and provide valuable insights for women seeking to take charge of their health.
Reduced Ovarian Cancer Risk with Total Hysterectomy
A total hysterectomy effectively removes the uterus and cervix, resulting in the elimination of the primary sites for the development of gynecological cancers, including uterine and cervical cancer. While this procedure significantly reduces the risk of these cancers, the presence of the ovaries still poses a potential risk for ovarian cancer.
It is important to note that undergoing a total hysterectomy alone does not eradicate the risk of ovarian cancer completely, as the ovaries may still be susceptible to cancerous growth. Therefore, it is crucial for women to discuss their individual risk factors and assess the need for additional preventive measures with their healthcare provider.
Assessing Ovarian Cancer Risk Factors
Various risk factors contribute to the likelihood of developing ovarian cancer, even after a total hysterectomy. Understanding these factors can empower women to make informed decisions and take proactive steps for their well-being. Let's delve into some of the key risk factors:
1. Age and Personal History
Age plays a significant role in determining the overall risk of developing ovarian cancer. Women over the age of 55 are more likely to develop this cancer. Additionally, individuals with a personal history of breast, uterine, or colorectal cancer may have a higher risk of ovarian cancer, emphasizing the importance of regular screenings and monitoring.
2. Family History and Genetic Factors
A family history of ovarian or breast cancer can significantly increase the risk of developing ovarian cancer. Moreover, certain inherited gene mutations, such as BRCA1 and BRCA2, are associated with a higher likelihood of ovarian cancer occurrence. Genetic counseling and testing can help identify these factors, allowing for appropriate risk management strategies.
3. Hormone Replacement Therapy (HRT)
Women who have undergone a total hysterectomy may be prescribed hormone replacement therapy (HRT) to manage menopausal symptoms. However, long-term use of estrogen-only HRT without progesterone has been associated with an increased risk of developing certain types of ovarian cancer. Discussing the benefits and potential risks of HRT with a healthcare provider is essential for informed decision-making.
4. BRCA1 and BRCA2 Gene Mutations
As mentioned earlier, certain gene mutations, such as BRCA1 and BRCA2, significantly elevate the risk of ovarian cancer. Individuals who inherit these gene mutations have an increased likelihood of developing ovarian cancer compared to the general population. Genetic testing and counseling can help identify individuals with these mutations, enabling them to take appropriate preventive measures.
Proactive Measures for Ovarian Cancer Risk Reduction
While certain risk factors for ovarian cancer may be beyond one's control, there are proactive measures that women can take to minimize their risk. These include:
1. Regular Health Check-ups
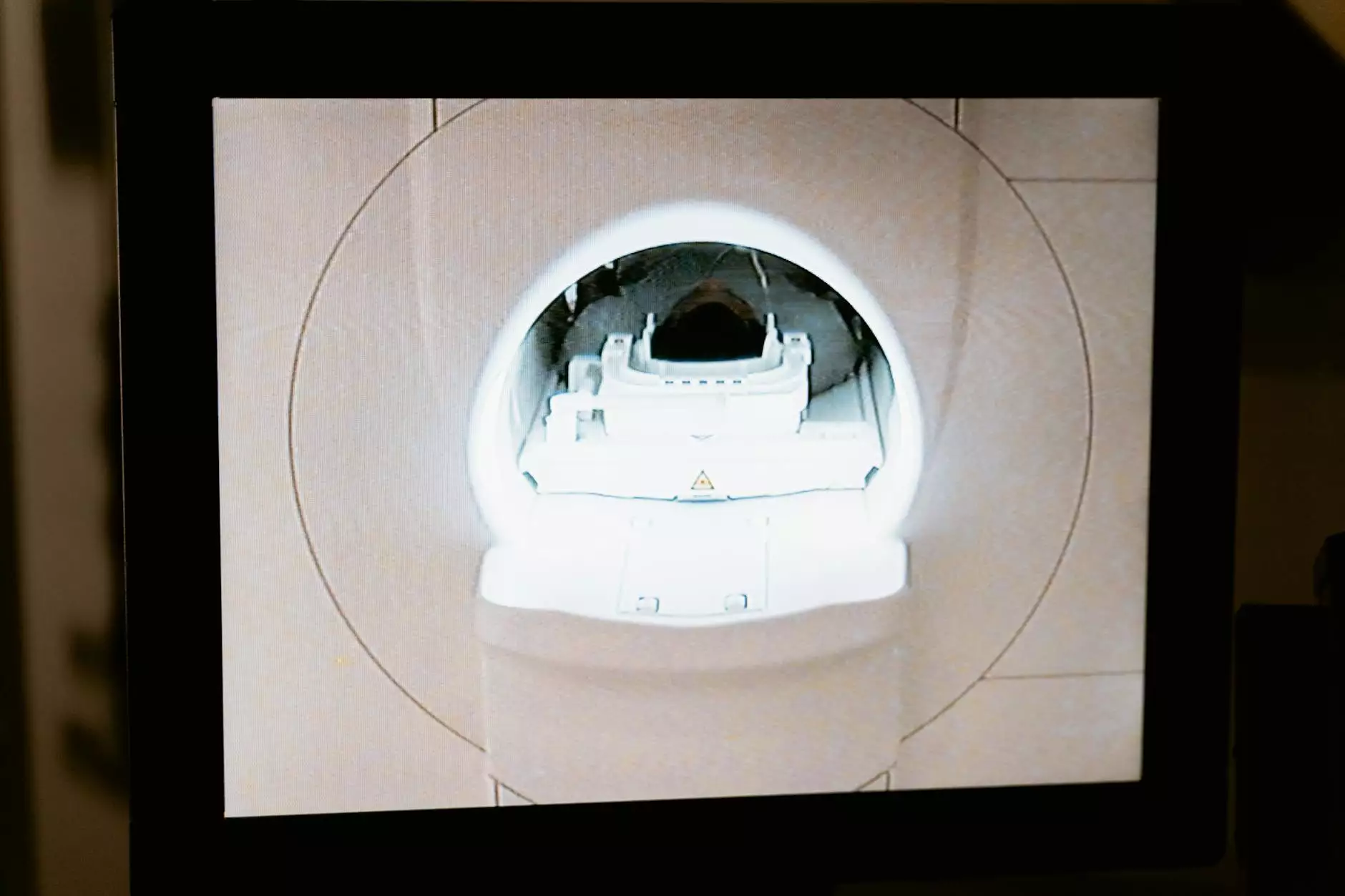
Regular visits to an Obstetrician & Gynecologist (OB/GYN) are crucial for early detection and management of any potential health concerns. Routine screenings, such as pelvic exams and ultrasound imaging, aid in the identification of any abnormalities or suspicious growths in the pelvic region.
2. Genetic Testing and Counseling
Individuals with a personal or family history of ovarian or breast cancer may benefit from genetic testing to identify specific gene mutations associated with increased cancer risk. Genetic counseling can provide valuable guidance in understanding these test results and making well-informed decisions regarding preventive measures.
3. Lifestyle Modifications
Adopting a healthy lifestyle can contribute to overall well-being and potentially reduce the risk of ovarian cancer. Regular exercise, a balanced diet rich in fruits and vegetables, and avoiding habits such as smoking and excessive alcohol consumption can help promote a healthy reproductive system.
Conclusion
Understanding the risk of ovarian cancer after a total hysterectomy is crucial for women's health and well-being. While a total hysterectomy significantly reduces the risk of uterine and cervical cancer, it does not eliminate the potential risk of ovarian cancer. By being aware of the various risk factors, seeking regular medical check-ups, and making informed decisions, women can take proactive measures to potentially reduce their risk and ensure optimal health.
risk of ovarian cancer after total hysterectomy